This post discusses a case study on a patient with systemic lupus erythematosus. A study carried out in the US showed that, on the average, it could take up to 5 years, or visit to as many as 5 to 10 different doctors, before an autoimmune disease [AID], lupus inclusive, could be properly diagnosed.
Below is an account of a case of lupus that was diagnosed in rural Benue, in a resource-poor facility, and how it could constitute a diagnostic “chameleon” mimicking almost anything.
I have decided to share it here for the following reasons:
– An alternate approach on my quest to create an awareness on autoimmune diseases, seeing that the initial approach was “too difficult” for the uninitiated to follow.
– To involve my readers in the diagnostic process, so that they may appreciate better the diagnostic dilemma associated with AIDs.
– To show that, contrary to what the uninitiated may think, a change in a diagnostic tag does not necessarily translate to “misdiagnosis” [in a sense of diagnostic incompetence] ; that an illness may bear different diagnostic tags at different stages in its evolution.
– To give an insight into the challenges facing the practice in rural settings.
– To stimulate an academic exercise in the mind of the initiated, and perhaps a debate.
Systemic Lupus Erythematosus-A case study
A 32 year old woman, X, presented as an emergency with complaints of flank pains, painful urination, gradual reduction in urine volume over one week, and subsequently, inability to make urine for 24 hours.
Before then, she had been having unexplained weight loss, fever, loss of appetite, and general body weaknesses for about 6 weeks, for which she went to a clinic, tested positive for HIV, and was started on ARVs [anti retroviral drugs for HIV]
Shortly after that, about 3 weeks before she developed inability to make urine, she developed diarrhoea and vomiting, and was still having those when she came to our hospital.
When she was examined, she had pains over both her kidneys [renal angle tenderness], and the blood pressure was so low [70/40mmHg] she was in shock.
At that point, the diagnosis was:
– Acute Renal Failure on a background of HIV stage 3 with :
1. Chronic Diarrhoea [with severe dehydration]
2. Acute Pyelonephritis [A kidney infection]
This diagnosis acknowledges that the woman’s kidney had failed, and that the identifiable risk factors that could have led to its failure are 1 and 2 above.
Initial recovery
Working with this diagnosis, she was rehydrated and brought out of shock, the kidneys were challenged as appropriate, and appropriate antibiotics were given to control the raging infection.
By the second day, the kidneys had “recovered,” and she had started making adequate urine. The diarrhoea had stopped, the fever was gone, and the pain over the kidney was subsiding.
A PCV done showed she had “shortage of blood,” and she was transfused.
A urinalysis done showed red, and white blood cells , and a granular cast in urine: all roughly in keeping with the working diagnosis.
MP for malaria was negative, and ESR was markedly elevated [118mm/hr: an unspecific indicator of inflammation]
[ Full Blood Count, Kidney function test, Liver function test, and abdominal scan were all requested for, but couldn’t be done due to a combination of financial constraint and unavailability of facilities required for those tests]
By the 5th day, appetite had improved remarkably, so much she could eat a horse. Also the renal angle and abdominal tenderness/pain had resolved completely. She could get out of bed without support, and go have her bath!
So, obviously I was on the right track. And we were talking about how to discharge her in a few days time.
Red flags
At about the 7th day, a day to her scheduled day of discharge [the plan was for her to go home, source for money, and go to the township and do the outstanding tests, and then come back to clinic with the results], she broke down again: fever, loss of appetite, nausea, vomiting, weakness, and mild leg swelling.
Even though the “kidney infection” had subsided, and she was apparently no longer in kidney failure, that initial insult must have caused some degree of damage in the kidney. That could explain the leg swelling, especially in the absence of cardiac symptoms [symptoms of a heart disease that could explain the leg swelling.]
The major worry though was the fever [38.8°c and above]. At this point, I needed a full blood count to know if I was dealing with an infectious process.
While waiting for the bread winner of the family to come back from a travel and provide financial assistance for the needed tests, we were using a combination of the strongest antibiotics we had, and antimalarials [all on credit], to treat the assumed infection.
3 days gone, and the fever was not responding to both. And to make matters worse, there was no evidence of an infectious focus: not the chest, the urinary tract, the central nervous system, nor the gut; all checked out fine, at least clinically.
Diagnosis
Having recurrent fever for up to 3 weeks [6 weeks in this case], and or having a fever that is not responsive to conventional therapy, meets the criteria for what is called “Fever of unknown origin” [FUO]. And in the setting of HIV, there are certain opportunistic infections that must be considered once one has such a fever. One of them is TB.
Given that she had been having weight loss, night sweats, loss of appetite, low back pain, contact with someone with chronic cough, and an ESR of 118mm/hr, all made TB look good. The fact that the AFB was negative, and Chest x-ray was not suggestive notwithstanding, more so where the CD4 count was low [In extrapulmonary TB, AFB my be negative, also a low CD4 may not allow for the characteristic chest findings]
Also, because she had a low CD4 count, was clinical stage 3, was apparently well but started getting worse when they started her on ARVs, all pointed towards a possibility of IRIS [ Immune Reconstitution Inflammatory Syndrome: a phenomenon in which commencement of HIV drugs paradoxically causes worsening of symptoms.]
So at that point, a new tentative diagnosis of “TB associated IRIS” [ the UNMASKING TYPE, with the component of SIRS (Systemic Inflammatory Response Syndrome) as Temperature was greater than 38 (39°C actually) , pulse was 120 beats per minute, and respiration was 30 cycles per minute] was made.
Right on track ?
With this diagnosis, ARVs were stopped temporarily, and while arrangements were being made for commencement of anti-TB drugs on clinical grounds, she was commenced on a steroid therapy with a resultant abrupt response, seemingly confirming the coexistence of an immune mediated process [in this case IRIS as diagnosed.]
By the second day, she was feeling much better, and the fever was gone.
However, the pharmacist had run out of patience, and stopped supplying drugs on credit, and the “bread winner” was yet to “show face.”
The “Flare”
Without the steroids to control the apparently raging inflammation, it flared up again. The fever was back, and with it came characteristic rashes, painless oral sores, blisters at sun-exposed areas of her skin, severe breathlessness with pleuritic chest pain [pain on intake of breath] , and features of heart failure.
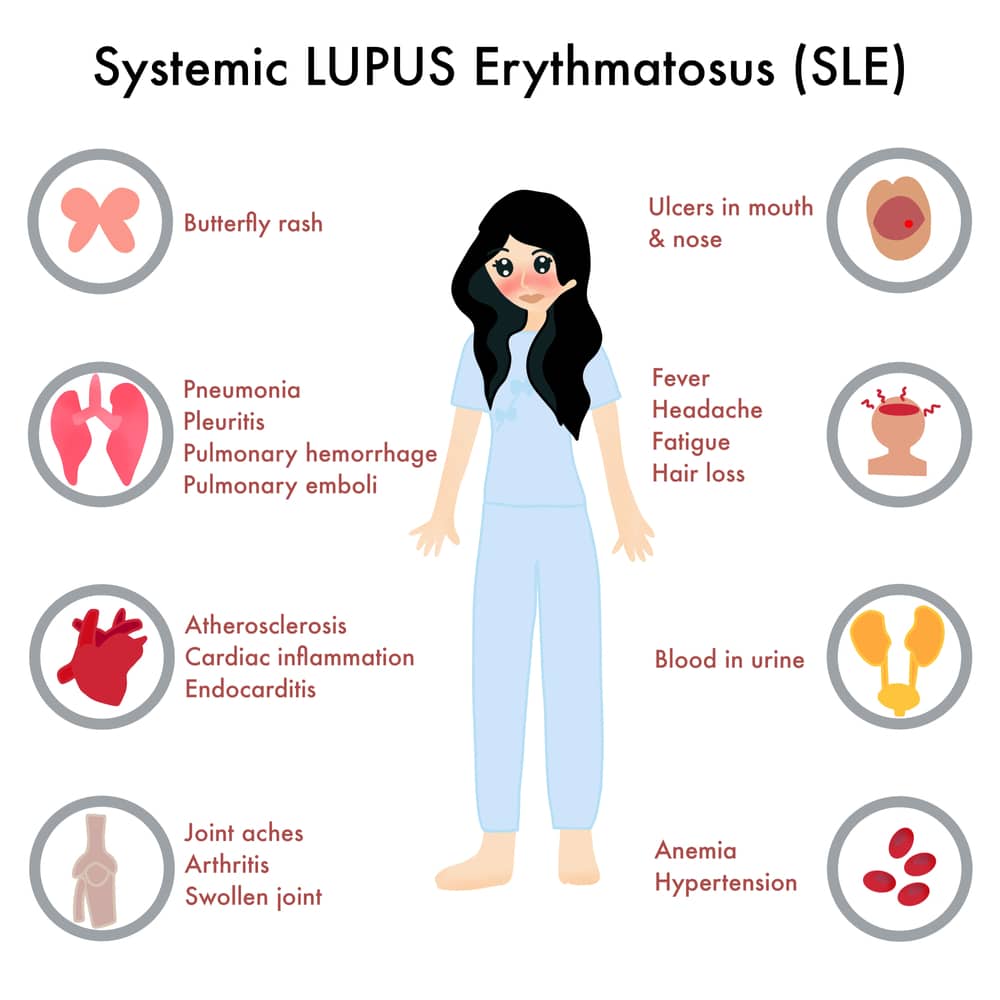
At this point, I knew I was dealing with something else: a multi systemic diseases, with an inflammatory basis, affecting the skin, serous membrane, kidney, lining of the lungs and heart, and the blood [as she was pale again, and was having evidence of “internal bleeding”].
I put a call across to Dr Obinna Ezeike, a senior registrar in NAUTH, and discussed the case extensively with him. At the end of the day, he said even though a disseminated TB unmasked by IRIS is not impossible, that he STRONGLY SUSPECTS a Lupus ‘flare up.’
At about the same time, the “bread winner” came around, and blood samples were taken and sent to a lab in the nearest township, some 40 minutes road distance away, for a kidney function test, and a full blood count.
The following morning, the results were out showing azotemia [impaired excretory function of the kidney as earlier suspected], and a full blood count picture showing anemia and low platelet count: similar to what is obtainable in Lupus.
Of the 11 criteria for diagnosing SLE, she scored a whooping 6, which is 2 points above what is needed for a diagnosis, even though she was yet to do the immunological tests!
Referral
She was promptly referred that morning.
Whether they went, or not, is another issue, as they were lamenting bitterly the probable cost of a teaching hospital admission, as they were leaving.
Secondly, the locals are so superstitious, they believe that a referral means “no hope;” that once “Ortwer gbim gbim” [me] refers, it means the person is going to die; that anything he cannot do, cannot be done elsewhere.
And no matter how hard you try to change this mentality, it is like pouring water on stone.
About the author
Dr Chibuike Joseph Chukwudum is a doctor who Studied Medicine and Surgery at Nnamdi Azikiwe University Awka. He is the former Medical Officer at Oakland specialist hospital,obosi.He also previously worked at Nnamdi Azikiwe University Teaching Hospital, Nnewi, Anambra State.


